COBRA Administration
CONSOLIDATED OMNIBUS BUDGET RECONCILIATION ACT
Staying up-to-date on the most recent changes in healthcare legislation and employment practices to keep your company compliant can be a daunting task for any HR professional. As an extension of your HR department, CPI is here to assist in ensuring you remain compliant with federal regulations under the Consolidated Omnibus Budget Reconciliation Act (COBRA).
COBRA Administration Services
Don’t spend your time tracking COBRA payments. Let us handle it! CPI can manage all required notifications to your employees, former employees, and/or their dependents, as well as answering any questions they may have. We will receive and apply payments and process elections on your company’s behalf, so your HR department can focus on other company needs and goals. Please review our COBRA services below:
Takeover
Once the employer and plans are setup, existing employee data will be imported and current COBRA participant activity. All existing COBRA participants will be sent takeover notices.
New Hires
General Rights Notices will be mailed as new employees are reported.
Qualifying Events
Specific Rights Notices will be mailed as events are reported (e.g. termination, divorce, loss of dependent status)
COBRA Elections
Elections will be processed with appropriate carrier(s) and the participant will be sent an election confirmation letter and payment coupons.
Premium Collection
Electing participants are provided with payment coupons and are sent communications regarding status of payments and coverage (e.g. partial payments, rate change notifications, NSF checks, etc.) Clients are reimbursed as payments are received and processed.
COBRA Terminations
The client and/or insurance agent will be notified when coverage should be canceled due to non-payment of premium or exhaustion of term. All required communications will be sent to the terminating participant.
Open Enrollment
All COBRA beneficiaries must be allowed the same open enrollment choices as similarly situated active participants. Upon request, open enrollment notification/materials will be mailed to active COBRA participants. *Additional fees may apply.
24-Hour Online Portal
Employers are able to enter participant information and view real-time data, add new hires or terminations, as well as run a variety of reports.
EDI Feeds
An EDI Feed is an automatic file feed that we setup to take the place of manual work for the employer and/or agent.
KEEPING UP WITH COMPLIANCE
What you need to know and how CPI can help.
COBRA REQUIREMENTS
--------
Employers of 20 or more employees must notify their newly enrolled employees of their rights under the Consolidated Omnibus Budget Reconciliation Act.
---------
Employers must offer continuation of coverage to employees and/or their dependents that experience a qualifying loss of coverage, all within designated timeframes.
FAQs
-
Who and What
The Consolidated Omnibus Budget Reconciliation Act of 1985, commonly referred to as COBRA, is a federal law that requires employers offering healthcare benefits to offer the option of continuing such coverage to qualified beneficiaries, at their own expense, who would otherwise lose their benefits due to employment termination, reduction in hours, or certain other events. COBRA applies to employers with 20 or more employees.
A qualified beneficiary is anyone covered under an employer’s group health plan on the day before an event that causes loss of coverage. Qualified beneficiaries include:
- Employees, including part-time employees
- Their spouses and dependents
- Retirees (unless they are eligible for Medicare)
- Partners in a partnership
COBRA coverage does not need to be offered to:
- An employee who is not yet eligible for the employer’s group health plan
- An eligible employee who declined to participate in the employer’s group health plan
- An individual who is enrolled for benefits under Medicare
Health plan, FSA and EAP benefits are COBRA eligible. Additional coverage may vary by state.
-
Where
The federal law applies to all states; additionally, state-specific laws may apply. These complex laws vary from state to state. When learning more about their state’s laws through their state labor agency or legal counsel, employers need to ask:
- Which benefit plans are covered?
- Which employers and benefit providers are subject to the law?
- Which employees are eligible to continue benefits under the law?
- Which events trigger continuation coverage (what are “qualifying events”)?
- Which notification requirements must employers comply with?
- How long can continuation coverage last?
- Under what circumstances can coverage be terminated?
-
When
Depending on the type of event and the qualified beneficiary, COBRA coverage could continue for 18 or 36 months after the date of the event or the coverage loss*:
- Termination of employment or reduction in hours: 18 months
- Qualifying events for reasons other than termination of employment or reduction in hours: 36 months
*Federal continuation time frames. State-specific time frames may apply.
-
Why
Events, known as qualifying events, that cause COBRA coverage are listed below.
- An employee’s voluntary or involuntary termination of employment, unless it is for gross misconduct. (While COBRA does not define misconduct, criteria to use if an employer is contemplating denying COBRA benefits due to misconduct are):
- There must be a connection between the offense and the employee’s job
- The employee must be able to understand the gravity of the misconduct
- The offense must be willful
- An employee’s reduction in employment hours (for example, from full-time to part-time)
- A covered spouse’s divorce or legal separation from an employee
- An employee’s death
- An employee’s entitlement to Medicare
- A covered dependent’s change in status (for example, reaching an age that no longer qualifies the dependent for coverage under the parent’s health plan)
- Active military duty when health coverage is not voluntarily maintained
- Failure to return to work at the end of family and medical leave where coverage was in effect at the beginning of the leave but was lost during the leave
- An employer’s bankruptcy
When a qualifying event triggers COBRA, in general, any plan offered to employees prior to the qualifying event must be offered. These plans can include: Healthcare, medical spending accounts, vision, dental, prescription drug, hearing, substance and alcohol abuse, and mental health.
COBRA coverage does not extend to life insurance, disability insurance, retirement plans, and vacation plans.
-
How
It is important that employers communicate to employees their right for continued benefits once a qualifying event happens. COBRA notification requirements include:
- Employers must notify covered employees and covered spouses of their initial rights under COBRA when they first join the plan.
- Employers must notify covered persons of their election rights to continue coverage after a qualifying event occurs.
- Employers have 30 days to notify the plan administrator (typically the insurance company) when a qualifying event occurs. In the event of divorce or change of status by a dependent, employers have 60 days. Once notified, the administrator has 14 days to notify the individual entitled to COBRA coverage.
- After an employee receives notification from an employer, the employee has 60 days to notify the employer that he or she wants coverage.
The employee generally pays the full cost of COBRA insurance premiums. The law allows the employer to charge 102 percent of the premium – the extra 2% is meant to cover administrative costs. If an employee receives extended COBRA coverage due to disability, the employer can charge 150 percent of the premium for months 19 through 29.
Federal law states that COBRA coverage can be terminated if premium payments are late. Payment is considered timely if it is made within 30 days after the due date or within a longer period set out under the plan. The due date must not begin before the first day of the coverage period. Additionally, when an individual chooses to take COBRA coverage, he/she has 45 days to make the first payment.
Most insurers want employers to pay in advance for coverage, and while that can complicate the process, the law states that employers must give individuals receiving COBRA coverage a 30-day grace period from the time the payment is due.
STAY CONNECTED
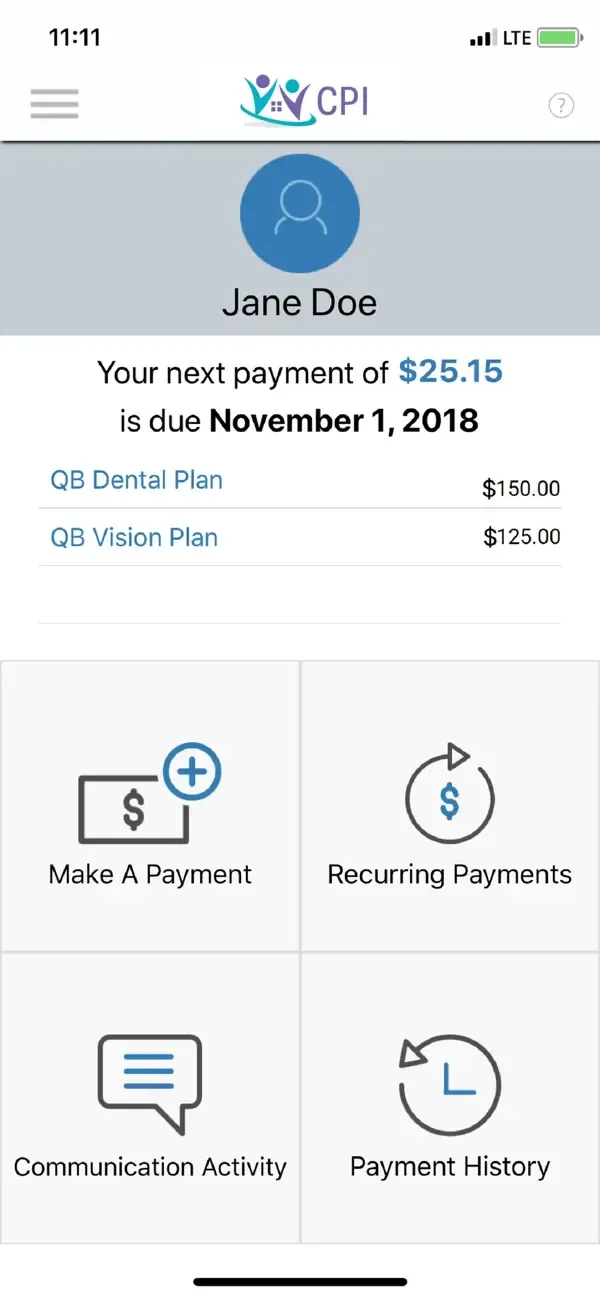


CPI Cobra + Direct Bill Mobile App
Stay up to date and worry free with the CPI’s COBRA & Direct Billing App! Manage your plans 24/7 through intuitive design and navigation while on the go. Powerful features of this app include (if supported by your account):
Plan Information
- Get visibility on payments made to your plan
- View notifications and receive messages from your administrator to stay up to date on your record
- Click to call or email Customer Service
Making Payments
- Make one-time payments when most convenient for you
- Schedule future and recurring payments to put you at ease
- Use your bank account or credit card
Elections
- Pick and choose the plan(s) that best suits you
- Avoid the hassle of paper by utilizing the latest in secure mobile payment technology
- View what you elected to better understand your coverage level, and make changes if needed
9 Definitions for COBRA, You Should Know
When it comes to COBRA administration, the terms, deadlines and steps for offering and administering COBRA are specific and time-consuming.
To help familiarize you with COBRA and the important specifics, we’ve compiled a list of key COBRA-related terms and their definitions you can use for reference.
Effective Date
The date when a participant's Cobra becomes active.
General Rights Notice
A written summary of COBRA rights and obligations. This notice is provided to new plan participants within 90 days of when group health plan coverage first begins.
Open Enrollment
A period of time, generally at the same time each year, when plans can be added or changed. Open enrollment is also the time when dependents can be added to plans and when participants are notified of any rate changes.
Participant
Any individual covered by a health plan through COBRA.
Summary Plan Description (SPD)
A document that explains the fundamental features of an employer’s group health plans, including eligibility requirements, contribution formulas, vesting schedules, benefits calculations and distribution options.
Premium
The amount a COBRA participant pays to extend coverage.
Qualified Beneficiary
An individual who is entitled to COBRA coverage because they were covered by a group health plan at least one day prior to experiencing a qualifying event.
Qualifying Event
An event that causes an individual to lose health coverage. There are seven types of qualifying events:
- Termination (except in the cases of gross misconduct)
- Reduction of hours
- Death of employee
- Divorce or legal separation from employee
- Loss of dependent status
- Medicare entitlement of employee
- Employer bankruptcy
Specific Rights Notice
A written notice outlining COBRA rights and obligations, including election forms. SRNs must be provided to all qualified beneficiaries within 14 days of receiving notice of a qualifying event.
AUSTIN, TX
LAFAYETTE, LA
NEW ORLEANS, LA
CINCINNATI, OH
LOS ANGELES, CA
We're here to help.
Customer Service Available
Monday-Friday: 7:30am–5pm, CST
7:30am -5pm EST, 8am -5pm PST
© 2022 All Rights Reserved | CPI
Website by BlinkJar Media